A groundbreaking discovery has been featured as the top story on the official website of Nature. For the first time, researchers have found that Pseudomonas aeruginosa, a superbug commonly found in hospitals, is capable of producing an enzyme that breaks down biodegradable plastics, allowing it to digest medical plastics.
This research, conducted by Brunel University London, was published in the Cell Reports, a sub – journal of Cell, on May 7, 2025. The paper is titled “Pseudomonas aeruginosa clinical isolates can encode plastic – degrading enzymes that allow survival on plastic and augment biofilm formation”.

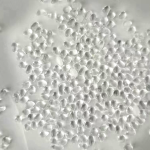
The research team isolated a strain of Pseudomonas aeruginosa, PA – W23, from the wounds of inpatients. This strain secretes an enzyme called Pap1 to break down polycaprolactone (PCL), a biodegradable plastic widely used in healthcare. This ability enables the bacteria to survive longer in hospital wards or within patients, making it more difficult to eliminate and more dangerous.
The research team noted that until now, all enzymes proven to degrade plastics have originated from environmental bacteria. This study, however, identified an enzyme with the same function in a common hospital pathogen, which may explain why these microorganisms persist in hospital environments. In the latest study, the team explored the genomes of common hospital pathogens and identified several microorganisms encoding enzymes homologous to known plastic – degrading enzymes. Among them, the clinical isolate of Pseudomonas aeruginosa, PA – W23, was found. The enzyme encoded by PA – W23 can degrade 78% of PCL plastic within 7 days. The team named this enzyme Pap1, and when the gene expressing this enzyme was knocked out, the Pseudomonas aeruginosa strain could no longer degrade plastic.
The study confirmed that this plastic – degrading ability allows the strain to survive using PCL as its sole carbon source. The team also discovered that when the strain comes into contact with plastic, the Pap1 enzyme increases the production of its biofilm. When a large amount of biofilm is produced, the bacteria’s antibiotic resistance is enhanced, leading to infections that are difficult to treat.
The researchers further conducted experiments on Galleria mellonella larvae. The results showed that in the presence of PCL implants, the Pseudomonas aeruginosa strain exhibits stronger pathogenicity. Additionally, the survival rates of larvae infected with Pseudomonas aeruginosa strains lacking the Pap1 enzyme were similar, regardless of the presence of PCL implants.
In conclusion, the clinical isolate of Pseudomonas aeruginosa, PA – W23, can degrade a medical – related plastic; the PA – W23 strain encodes the novel Pap1 enzyme responsible for plastic – degrading activity; and it can utilize plastic as a carbon source for growth. These findings indicate that the plastic – degrading ability of the Pap1 enzyme can enhance the formation of bacterial biofilms and pathogenicity. Given the central role of plastics in healthcare, the plastic – degrading ability of hospital bacteria should be an important consideration in the future.